If we listened to and believed some of the comments about small-diameter implants (SDIs) (or “mini” implants) that we hear coming from some areas of surgical dentistry, we would be led to think that these devices simply do not work. However, the truth is diametrically opposed to what some are saying, and it has been our observation that some of the most severely negative comments come from dentists who have never placed SDIs.
This article includes: the definition of “mini” or SDIs; a discussion of the evolution of SDIs, including their clearance by the US Food and Drug Administration (FDA) and research support; reasons for SDI use instead of conventional diameter implants; the indications for SDI use; and suggestions on how to use them successfully.
THE EVOLUTION OF THE SMALL-DIAMETER IMPLANT CONCEPT
There is no question among dentists that root-form implants, 3.0 mm in diameter and more, are one of the most successful and important additions to clinical dentistry in the entire history of dentistry. The FDA cleared these conventional-diameter root-form implants for clinical use in 1976. Millions of conventional-diameter implants have been placed for more than 4 decades, and their cumulative success rate of around 95% is impressive. In many situations, it has been our experience that the conventional prosthodontic portion of implant treatment fails faster than the properly integrated root-form implants themselves.
In the early 1990s, some innovative practitioners started using SDIs (up to 2.9 mm in diameter) for long-term use in situations with insufficient bone. At that time, SDIs were then considered to be for transitional use only. Also, orthodontists began using SDIs, also known as temporary anchorage devices, for anchorage for difficult tooth movement situations. It soon became obvious to those practitioners that properly placed SDIs were working adequately.
As a result of their obvious clinical success, SDIs were cleared by the FDA “for long-term intrabony applications” with the help of the Imtec company in 1997. Subsequently, numerous other SDI brands have received similar FDA clearance. Thousands of these SDIs are now in successful restorative use with a reported 91% to 97% survival rate. Numerous surveys, testimonials, research projects, and satisfied dentists and patients attest to that fact.1-6 Many more positive references are available in the restorative, prosthodontic, and orthodontic literature.
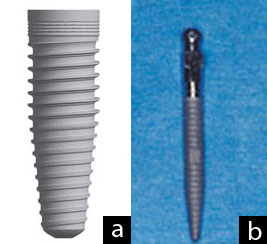
- Images 1a and 1b. A typical conventional diameter implant has a blunt end necessitating cutting a hole in the bone for placement. A typical small-diameter implant (SDI) has a screw configuration that expands minimal bone on placement. This difference is one that allows SDIs to be placed in bone as thin as 3 to 4 mm in the facial lingual dimension.
WHY USE SMALL-DIAMETER IMPLANTS IF CONVENTIONAL DIAMETER IMPLANTS ARE SO SUCCESSFUL?
Both of the authors of this article are prosthodontists who place both conventional and small-diameter root-form implants. The following are their observations on the desirability of SDI use compared to conventional diameter implant use.

- Image 2. SDIs (Imtec a 3M ESPE company) placed in a mandible model. Small spheres on the implants and rubber washers in housings in the denture support and retain the denture.
Inadequate Bone Quantity
Conventional diameter implants, averaging about 3.5 mm in diameter, require minimally about 6 mm of bone in a facial-lingual dimension, and about 10 mm of bone in a crestal-apical dimension, for uncomplicated placement without grafting. Some patients accept the overall implant concept, but they have inadequate bone quantity and do not want to have significant bone grafting accomplished.
SDIs can be placed in as little as 3.0 mm of bone in a facial-lingual dimension and 10 mm of bone in a crestal-apical dimension. In fact, often bone 3 or 4 mm in a facial-lingual dimension is ideal, because the cortical bone plate on the facial has nearly approximated the lingual cortical plate, and this dense bone holds the SDI securely. Some experienced implant surgeons may question this, until they consider the fact that the SDI is usually a “screw,” expanding bone instead of cutting it away.

- Image 3. Atlas (Dentatus) implants placed in a mandible model. Small spheres on the implants and soft denture reline material in the denture support and retain the dentures.
Inadequate Financial Resources
Some patients have inadequate bone, accept the implant concept, accept the need for extensive bone grafting, and they are ready to accept the treatment with the following exceptions: the cost of the grafting is too high, the expense of the restorative treatment is high, and conventional diameter implant treatment is denied. SDIs frequently solve this challenge, as stated in the previous point.
Compromised Physical Condition
Many physically debilitated patients do not have the ability to tolerate conventional diameter implant placement, but they can tolerate the simple, few-minute placement of SDIs without a flap. Recent research has shown that flapless implant placement may accelerate osseointegration and produce quicker healing. Debilitated persons can benefit from these simple procedures.

- Image 4. Zimmer (Sterngold) implants placed in a mandible model with ERA attachments on the implants. Reciprocal ERAs in the denture base support and retain the denture.
Major Uses of Small-diameter Implants
SDIs are listed in the Table in approximate order of decreasing frequency of use, as noted in the previously referenced articles, our own use patterns, and our observation of other practitioners.
If SDIs were used only for patients with edentulous mandibles, roughly 35 to 40 million edentulous patients in the United States alone would have better fitting and retained complete dentures. These implants are so easy to use in most edentulous mandibles that it is upsetting to us that they are not used more in the profession for the indications noted above
WHY DO SOME DENTISTS STATE THAT SMALL-DIAMETER IMPLANTS\ ARE NOT SUCCESSFUL?
Many of the same surgical dentists now condemning SDIs stated 40 years ago that conventional root from implants would not work. It appears that their opinion is that anything new is automatically bad! SDIs are new, but they are proving themselves.
This section is probably the most important part of this article. Some SDIs fail. We have experienced a few failures ourselves over the past 9 years of use. These failures were almost always related to one or more of the following errors:
- Too much thickness of the soft tissue. If the ratio of the coronal portion of the SDI to the portion placed in the bone is excessive, a long lever arm is present. This situation stresses the SDI and may lead to failure of the implant. If the soft tissue, through which the SDI is to be placed, is thicker than about 2 mm, it should be reduced by taking a wedge of tissue from the coronal portion of the ridge. This can be done before the implants are placed, allowing for adequate healing, or at the time of implant placement. This surgery may be done with a scalpel, or some lasers may be used around implants to accomplish this task without causing damage to the implant osseointegration potential.
- Improper parallelism of implants. SDIs should be as parallel as possible. If these implants are much more than 15° from parallelism, technical difficulty at placement of the prosthesis and subsequent potential clinical failure can be anticipated.
- Inadequate preoperative radiographs. Poor bone is commonly present in some areas of edentulous patients. We discourage using only 2-dimensional conventional panoramic radiographs, because you cannot determine the quality or quantity of the bone in a facial-lingual dimension. Coarsely trabeculated bone is not appropriate for SDIs. The more dense the bone, the better. To determine the density of the bone, facial-lingual oriented radiographs are strongly suggested. These include tomograph or cone beam radiographs. Most communities now have accessibility to some form of the suggested facial-lingual orientation radiographs at moderate cost.
- Poor bone density in the posterior maxillary tuberosity areas. Usually, the dense Type I bone of the resorbed anterior mandible is excellent for SDIs. The worst bone, contraindicated for SDI placement by most experienced practitioners is the posterior maxillary tuberosity, with its porous type IV bone. A careful analysis of the density of the bone in any other part of the oral cavity is suggested, as they too may have poor bone density contraindicating SDIs.
- Too few SDIs are often placed. It has been suggested in both empirical and research reports that the minimal number of SDIs for edentulous mandibles is 4, evenly spaced from the left canine area to the right canine area. This is double the minimal number of implants suggested for conventional diameter implants. The ratio appears to be 2 SDIs where one conventional diameter implant would usually be used. Some companies are suggesting 6 SDIs instead of 4 for edentulous maxillas, evenly spaced from the canine area to the opposite canine areas. However, the more dense the bone, the fewer SDIs that are needed.
- SDIs are too short. The most popular average length for SDIs is 13 mm. It appears from both clinical observation and research that this is a predictable and successful length. The implants must be used in adequate bone, according to the literature of reported successful use of thousands of SDIs and to the discussions with manufacturers about clinician reports to them.
- Poorly adjusted occlusion, or loading the implants too soon. Most SDIs are loaded immediately on placement. Occlusion needs to be adjusted perfectly on placement of the prosthesis. Allowing heavy occlusion to traumatize these small implants is asking for early failure. If questionable bone quality or quantity is present, soft denture reline material may be placed in the denture around the area of the implants for several weeks to ensure that they have optimum time for initiation of osseointegration.
| Table. Use of SDIs in Approximate Order of Decreasing Frequency of Use |
| •Edentulous mandible •Removable partial denture •Edentulous maxilla (this use has higher failure rate than edentulous mandibles) •Augmentation of fixed prosthesis •Sole support of fixed prosthesis •Salvage of previously made prosthesis |
SUMMARY AND CONCLUSION
SDIs that are treatment planned correctly, placed and loaded properly, and are within a well-adjusted occlusion, are working in an excellent manner for the patients described in this article. It is time for those practitioners unfamiliar with SDIs and their uses to discontinue their discouragement of this technique. SDIs are easily placed, minimally invasive, and a true service to those patients described. They do not replace conventional diameter implants; however, they are a significant and important augmentation to the original root-form implant concept. There is obvious evidence of the growing acceptance of small-diameter implants by both general practitioners and specialists.
References
- Bulard RA, Vance JB. Multi-clinic evaluation using mini-dental implants for long-term denture stabilization: a preliminary biometric evaluation. Compend Contin Educ Dent. 2005;26:892-897.
- Clinical Research Associates. Small-diameter “mini” implants—user status report. CRA Newsletter. 2007;31:1-2.
- Griffitts TM, Collins CP, Collins PC. Mini dental implants: an adjunct for retention, stability, and comfort for the edentulous patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:e81-e84.
- Morneburg TR, Pröschel PA. Success rates of microimplants in edentulous patients with residual ridge resorption. Int J Oral Maxillofac Implants. 2008;23:270-276.
- Shatkin TE, Shatkin S, Oppenheimer BD, et al. Mini dental implants for long-term fixed and removable prosthetics: a retrospective analysis of 2514 implants placed over a five-year period. Compend Contin Educ Dent. 2007;28:92-99.
- Vigolo P, Givani A. Clinical evaluation of single-tooth mini-implant restorations: a five-year retrospective study. J Prosthet Dent. 2000;84:50-54.
Dr. Christensen is currently a practicing prosthodontist in Provo, Utah. His degrees include DDS, University of Southern California; MSD, University of Washington; and PhD, University of Denver. He is a Diplomate of the American Board of Prosthodontics, a Fellow and Diplomate in the International Congress of Oral Implantologists, a Fellow in the Academy of Osseointegration, American College of Dentists, International College of Dentists, American College of Prosthodonists, Academy of General Dentistry (Hon), Royal College of Surgeons of England, and an Associate Fellow in the American Academy of Implant Dentistry. Drs. Gordon and Rella Christensen are co-founders of the nonprofit Gordon J. Christensen CLINICIANS REPORT (previously CRA). He has presented more than 45,000 hours of continuing education throughout the world and has published many articles and books. He can be reached at (801) 226-6569 or via e-mail at [email protected].
Disclosure: Dr. Christensen reports no conflicts of interest.
Dr. Child is the CEO of CR Foundation, a nonprofit educational and research institute (formerly CRA). He conducts extensive research in all areas of dentistry and directs the publication of the Gordon J. Christensen CLINICIANS REPORT, and other publications. Dr. Child graduated from Case Western Reserve University School of Dentistry, completed a prosthodontic residency at LSU, and maintains a private practice at the CR Dental Health Clinic in Provo, Utah. He is also a Certified Dental Technician through National Board of Certification in Dental Lab Technology. Dr. Child lectures nationally and copresents the “Dentistry Update” course with Drs. Gordon and Rella Christensen. He lectures on all areas of dentistry, with an emphasis on new and emerging technologies. He maintains membership in many professional associations and academies. He can be reached at (801) 226-2121 or via e-mail at [email protected].
Disclosure: Dr. Child reports no conflicts of interest.
