INTRODUCTION
“Communication is key.”
“It’s all about communication.”
Sound familiar?
The Merriam-Webster Dictionary describes communication as “a process by which information is exchanged between individuals through a common system of symbols, signs, or behavior.” Communication is a 2-way street. It involves a verbal exchange that includes speaking or writing and, importantly, listening. After the dentist writes on a prescription pad, it is then up to the dental laboratory team to understand exactly what the dentist wants. The clinician envisions how the restoration should look, then often communicates details verbally to the lab technician as well. The lab technician then interprets all the promulgated information and creates the restoration or prosthesis that he or she understands to be what the dentist and patient desire. To a large degree, the successful execution of this process depends on the clinical skill of the dentist, as well as the technical skill of the technician. And fundamental to success is the need for accurate communication between the doctor and the lab team. When such communication is optimized, it becomes collaboration. In the ever-expanding schema of digital dentistry, communication and collaboration both rely increasingly on another critical component: data.
Expectations vs Communication
Restorations are created to restore form and function and provide aesthetic outcomes that meet the needs and expectations for the dentist and the patient. By reliance on an aggregate of these components, the essence of communicating with a dental laboratory technician is for him or her to reproduce a restoration or prosthesis exactly to the specifications the restorative dentist requested, including tooth shape, size, and position within the dental arch; occlusal relationship; emergence profile; interproximal contacts; and incisal edge position.


The aesthetic outcome is dependent on communicating color (chroma, hue, and value), translucency, and surface texture. The underlying challenge for the dentist is to determine all of these parameters accurately and then be able to successfully communicate the details and expectations for the patient case. The challenge for the lab team is to then understand exactly what the dentist is asking for and successfully implement the information received in the restorative product.
In the traditional way of doing things, the dentist will provide the lab technician with a written prescription describing what is expected. Of course, the detailed prescription needs to be accompanied by impressions, diagnostic casts, a bite registration, face-bow records, and clinical photos.
Doctor-Technician Communication
The digital approach now has the ability to optimize what, and how, relevant clinical information (STL files, DICOM files, digital photos, and/or videos) gets to the lab team and how the instructions and directions for restorative fabrication take place.
A substantial body of literature has been published on individual aspects of digital workflows in the prosthetically driven implant placement clinical setting, including several recent systematic reviews.1-4 In general, these reviews report an overall time reduction in providing multi-unit prostheses. Joda et al4 state the need for more studies focusing on patient-reported outcome measures in this area. Abduo and Elseyoufi3 reviewed studies that included 12 intraoral scanning systems and identified considerable variability among them. They caution that intraoral scanners are vulnerable to inaccuracies, especially in long-span scanning applications.3 An in vitro comparative study by Amin et al5 identified a superior accuracy of digital impressions using intraoral scanners compared to conventional impressions for full-arch prostheses. Literature addressing the advantages of all aggregate facets of a digital workflow are scarce; the author published an initial report on the initial promise of digital dentistry in 2016.6
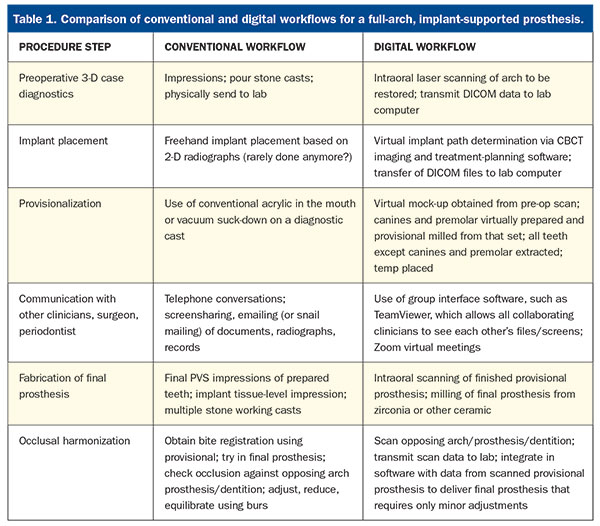
In a digital workflow, communication between the doctor and the lab team becomes much more transparent, accessible, and collaborative to both individuals. Table 1 presents contrasting steps between conventional and digital workflows.
Digital Workflow
• Diagnostic digital wax-up:
Using a laser introral scanner (eg, TRIOS [3Shape]), the dentist will send scans of the existing dentition to be restored to the lab technician who then creates the proposed restorations in the virtual 3-D model using dental design software. The dentist then views the design remotely and has an exchange with the technician about any aspects of the design. It can then be improved or modified, and the process continues until both are satisfied with the results.
• Cone-beam computed tomography (CBCT):
Central to the theme of digital dentistry is the capability for 3-D imaging afforded by CBCT scanning. Such scans provide the core of data accessible to every other virtual modality of treatment planning. Although there are some software incompatibility issues, CBCT scans form the basis for accurate digital implant placement and restoration.








screw-retained zirconia prosthesis.
In the case of smile design, the digital wax-up can be printed or milled using a variety of materials and sent to the dentist to be further reviewed and, if desired, tried in the patient’s mouth. Provisionals can then be fabricated from the approved design. This works extremely well in the case of full-mouth reconstruction. The patient will wear the provisional restoration for an appropriate amount of time. When all form, function, and aesthetic parameters have been addressed, the provisional result can be scanned in the patient’s mouth, and then the definitive restoration can be copied exactly from that provisional. We have followed this process in our practice for a number of years with numerous cases and consistently find that only minimal adjustments are necessary at the final seating appointment.
Summary of General Steps in a Digital Workflow
- Obtain a preoperative CBCT and intraoral scans of the patient
- Print or mill the approved proposal
- Insert
- Scan and copy
- Fabricate the definitive restoration
Digital Orthodontics
Orthodontists and restorative dentists can treatment plan using a variety of software platforms. These include Invisalign (Align Technology), SureSmile (Dentsply Sirona), and Reveal Clear Aligners (Henry Schein), just to name a few. These software technologies allow the dentist to send photos, radiographs, CBCT and intraoral scans, and other digital files in an electronic prescription with specific instructions. Proposed tooth and root movements are again made available for the clinician to modify, if needed, and approve. For fixed orthodontics, wires can be pre-bent robotically by the lab team and, in the case of aligners, they are all fabricated from the digital design.
Digital imaging of the airway can also provide diagnostic information on potential sleep-related breathing disorders.
Challenges
Going digital doesn’t simply mean “buying a scanner.” Rather, it involves adopting new workflows, and this requires a commitment from the dentist, as well as the entire team, in order to obtain a level of mastery that, in turn, creates consistency, reliability, and clinical accuracy. Proper technique and proficiency with the equipment are necessary to reliably scan and relay the resulting digital files to the lab team.
As is frequently the case with medical imaging software, compatibility issues can pose obstacles to the digital workflow. Each manufacturer uses some proprietary file format that may or may not require the lab to have the same licenses to view and work with those files. While there is some interoperability between different scanners and the design software in the laboratory (eg, 3Shape and exocad Dental CAD), challenges persist in sharing designs across different platforms.
Solutions
Digitally communicated workflows have become ubiquitous in implant planning for restoratively driven implant placement. The sharing of STL and DICOM files on a variety of platforms, such as Dropbox, has improved clinical outcomes in many ways. It has led to successful communication not only between the dentist and the lab team, but also between the lab team that fabricates the surgical guides, the clinician who places the implants, and the dentist responsible for placing the restorations. For example, DDx Solution (Henry Schein) allows for the exchange of lab data from Dentrix to the lab team. Other manufacturers’ platforms, such as Planmeca Romexis, Dentsply Sirona Connect, NobelGuide, or Straumann DTX, enable more-seamless communication.
For case discussions, dentists and their lab teams can collaborate with widely used communication software such as Zoom, GoToMeeting, LogMeIn, and others. Group interface software, such as TeamViewer, can also optimize digital collaboration among restorative and specialty clinicians by allowing them to view the files and screens of all collaborators.
CASE REPORT
Diagnosis and Treatment Planning
A healthy 57-year-old man with no significant medical conditions, no known drug allergies, and taking no medications presented for a full rehabilitation of his mandibular arch. He had recently undergone an immediate-load, full-arch, maxillary rehabilitation and wanted to have a similar treatment on his lower arch. A traditional all-on case would have required significant alveolar bone reduction, which would have limited the overall A-P spread of the implants or reduced the implant sizes. The patient did not want to wear an interim removable prosthesis, so the decision was made to stage the case with a transitional fixed bridge on 3 existing teeth as abutments while the implants fully integrated.
Clinical Protocol
Implants were placed in the mandible and prepared to support a transitional provisional fixed prosthesis that enabled the patient to avoid a removable provisional prosthesis. The preparation and planning allowed for an efficient appointment in which the extraction of the anterior teeth, the guided placement of all 6 implants in one appointment, and the insertion of the fixed provisional took place in an uneventful workflow.
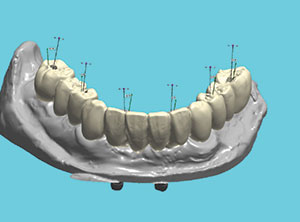
Figure 1 shows a pre-op scan image of the mandibular dentition in occlusion with the existing maxillary prosthesis to digitally capture the vertical dimension of occlusion. Figure 2 shows a frontal CBCT image of hopeless anterior teeth resulting from pronounced osseous defects. Figure 3 shows a virtual image produced from a scan of the remaining mandibular dentition after the virtual extraction of mandibular incisors and premolars, with teeth Nos. 22, 27, and 29 prepared to support the virtually milled provisional.
A computer rendering of the proposed prosthesis in occlusion with the existing maxillary prosthesis, consistent with restorative-driven implant treatment planning, is shown in Figure 4.
Next, the workflow used the first of 2 digitally milled surgical guides to place the first 2 implants in position Nos. 19 and 31 (Figure 5). The second surgical guide (Figure 6) was then placed over implants in position Nos. 19 and 31 and prepared teeth Nos. 22, 27, and 29 after the extraction of teeth Nos. 20, 23, 24, 25, 26, and 28. The remaining 4 implants were then placed in position Nos. 20, 23, 26, and 30. None of the implants were loaded at the time of placement. All implants were placed using full facial and lingual flap reflection at the same appointment.
Next, the fixed provisional was placed using abutment Nos. 22, 27, and 29 (Figure 7). A panoramic radiograph showing 6 implants immediately after placement, and the 3 remaining abutment teeth to support the immediate fixed PMMA provisional, is pictured in Figure 8. Figure 9 shows a panoramic radiographic view of the provisional abutments attached to the implants immediately after the extraction of teeth Nos. 22, 27, and 29.
After 3 months of healing to allow for osseointegration, the 6 implants were uncovered, had scan bodies placed, and were scanned at the fixture/tissue level. Figure 10 shows virtual relative angulation of the screw access holes and implants. Teeth Nos. 22, 27, and 29 were virtually extracted, and a full-arch, mandibular, implant-supported provisional was fabricated. Next, teeth Nos. 22, 27, and 29 were extracted, and the screw-retained provisional was secured to the 6 implants (Figure 11). Time was allowed for tissue healing, and a definitive screw-retained, milled zirconia prosthesis was placed (Figure 12).
CLOSING COMMENTS
The case example above serves to demonstrate how complex implant restorative dentistry can be achieved. This treatment provided the patient with immediate function on existing teeth or? integrated implants in fewer appointments and with greater predictability using a digital workflow as compared to the risks and limitations associated with a traditional-load all-on case dentist-lab team exchange.
Acknowledgment:
The author extends his appreciation to Dr. Evan Chafetz, DMD, oral-maxillofacial surgeon, Scarsdale, NY, and Robert Schulman, DMD, prosthodontist, White Plains, NY.
References
- Lo Russo L, Caradonna G, Biancardino M, et al. Digital versus conventional workflow for the fabrication of multiunit fixed prostheses: a systematic review and meta-analysis of vertical marginal fit in controlled in vitro studies. J Prosthet Dent. 2019;122:435-440.
- Mühlemann S, Kraus RD, Hämmerle CHF, et al. Is the use of digital technologies for the fabrication of implant-supported reconstructions more efficient and/or more effective than conventional techniques: a systematic review. Clin Oral Implants Res. 2018;29(suppl 18):184-195.
- Abduo J, Elseyoufi M. Accuracy of intraoral scanners: a systematic review of influencing factors. Eur J Prosthodont Restor Dent. 2018;26:101-121.
- Joda T, Derksen W, Wittneben JG, et al. Static computer-aided implant surgery (s-CAIS) analysing patient-reported outcome measures (PROMs), economics and surgical complications: a systematic review. Clin Oral Implants Res. 2018;29(suppl 16):359-373.
- Amin S, Weber HP, Finkelman M, et al. Digital vs. conventional full-arch implant impressions: a comparative study. Clin Oral Implants Res. 2017;28:1360-1367.
- Kaye G. Restorative digital dentistry, part 1: the journey to new paradigms. Dent Today. 2016;35:22-27.
Dr. Kaye graduated from the Columbia University School of Dental Medicine, where he received awards in endodontics, prosthodontics, and geriatric dentistry. He has practiced comprehensive dentistry since 1993 and has built successful multispecialty group practices in and around New York. He is a graduate of the Dawson Academy of Comprehensive Dentistry and has published and lectured on ceramics, occlusion, and the adoption of digital dentistry. He consults with dentists, dental schools, and manufacturers on all aspects of digital dentistry. Dr. Kaye serves as the digital editor for Dentistry Today. He can be reached at [email protected].
Disclosure: Dr. Kaye reports no disclosures.
